In the pathophysiology of Sickle cell anemia or Sickle cell disease (SCD), we learn that it is a systemic disorder caused by a mutation in the gene encoding the β chain of hemoglobin.
This mutation leads to the production of sickle hemoglobin HbS. Sickled red blood cells were first observed in 1910 by JB Herrick in a Black West Indian student.
Introduction to pathophysiology of sickle cell anemia
Sickle cell anemia or Sickle cell disease is the result of a single base-pair change, thymine for adenine, at the sixth codon of the beta gene.
in which the change encodes Valine instead of glutamine in the sixth position on the beta-globin molecule.
Beta globin haplotypes are the different DNA structures associated with the sickle gene are identified by a pattern of restriction enzyme sites.
Therefore, it is important to note that the HbS gene is prevalent in malaria-endemic regions, distribution is however worldwide, with the greatest incidence in tropical Africa.
It occurs in the USA, Middle East, India, the Caribbean, South and Central America, Turkey, and throughout the Mediterranean region.
A 2009 study carried out in Nigeria showed that 2-3% of Nigerian newborns are homozygous.
Incidence in the general Nigerian population is 1:300 with Frequency of the S gene in Nigeria is about 25% Mode of inheritance= autosomal recessive.
Pathogenesis and pathophysiology of sickle cell anemia
The hemoglobin molecule (alpha and beta-globin subunits) picks up oxygen in the lungs and releases it when the red cells reach peripheral tissues, such as the muscles in Sickle cell anemia or Sickle cell disease.
And also, normal red cells maintain a basic disc shape, whether they are transporting oxygen or not but the case is different with sickled hemoglobin.
Sickle hemoglobin exists as isolated units in the red cells.
when they have oxygen bound, Whereas sickle hemoglobin releases oxygen in the peripheral tissues, however, the molecules tend to stick together and form long chains or polymers (polymerization).
These rigid polymers interact with the cell and cause it to bend out of shape Polymerized sickle hemoglobin does not form single strands.
But the molecules group in long bundles of 14 strands each that twist in a regular fashion, much like a braid.
In Sickle cell anemia or Sickle cell disease, most distorted cells are simply shaped irregularly, a few have a cresent-like appearance under the microscope.
These cresent-like or “sickle-shaped” red cells gave the disorder its name. A single red cell may traverse the circulation four times in one minute. Sickle hemoglobin undergoes repeated episodes of polymerization and depolymerization (sickle-unsickle cycle).
This cyclic alteration in the state of the molecules damages the hemoglobin and ultimately the red cell itself.
Diameter of RBC =7microns
Diameter of capillaries =3microns
Summary on the sickle cell anemia,
In Sickle cell anemia or Sickle cell disease Polymers tend to grow from a single start site (nucleation site) and often grow in multiple directions. Star-shaped clusters of hemoglobin S polymers develop commonly.
Sickling occurs at the venous end of capillaries whereas unsickling occurs at the arterial end.
Two essential pathological processes arise from sickling: Haemolysis and vaso-occlusion
The pathological features of SCD relate to the shortened life span of the sickled blood cells, (16-20 days rather than a lifespan of 120 days in normal red cells) which leads to hemolytic anemia
The mechanism is likely to be responsible for complications such as pulmonary hypertension and stroke.
Sickled cells directly cause Small vessel occlusion

Vaso-occlusion is the major cause of morbidity and mortality in sickle cell anemia, accompanied by occlusion of blood vessels followed by ischemia or infarction in various tissues, leading ultimately to progressive end-organ damage.
The process of vaso-occlusion
It was first thought that hemoglobin S polymerization resulted in the entrapment of sickled, poorly deformable erythrocytes that mechanically blocked small-caliber vessels.
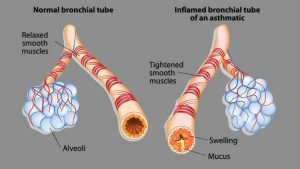
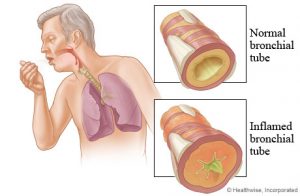
Damage similar to that seen in patients with the atherosclerotic vascular disease has been seen in the large cerebral vessels of patients with Sickle cell anemia or Sickle cell disease, including intimal hyperplasia, and fibroblast and smooth muscle proliferation.
It will be of great importance to consider these terms [CRISES]; Vaso-occlusive, Haemolytic, Aplastic, and Acute sequestration.
VASO-OCCLUSIVE CRISIS
This crisis is due to obstruction of blood flow in the smaller venules, capillaries and even in medium-sized or large arteries, as a result of the increased viscosity and sludging associated with sickling.
The increased adhesiveness of sickled reticulocytes worsens occlusion. Vaso-occlusion is the pathophysiologic basis of most of the clinical.
HAEMOLYTIC CRISIS
Hemolytic crisis makes RBCs are broken down at a more rapid rate than during the steady-state of the disease, it is precipitated by malaria and bacterial infections.
Features include:
*Severe anemia, Cardiac failure
*Jaundice, hepatomegaly.
*Encephalopathy-seizures, altered sensorium
*The terms ‘ hemolytic’ and ‘hyper haemolytic’s are often used interchangeably, but the latter technically refers to the co-existence of SCA and G6PD[glucose 6-phosphate dehydrogenase deficiency].
APLASTIC CRISIS
There is a shut down of the bone marrow which is usually limited to the red blood cell precursors, making the patient become profoundly anemic and may go into high-output cardiac failure.
Anemia reoccurs after blood transfusions until the crisis is over, Several viruses are associated with this syndrome most especially parvovirus B19.
ACUTE SEQUESTRATION
The Pooling of blood in the spleen is a frequent occurrence in children with sickle cell anemia, particularly in the first few years of life, resulting in splenic sequestration crisis.
They are often associated with viral or bacterial infections; acute chest syndrome occurred in 20% in one series.
The usual clinical manifestations are sudden weakness, pallor, tachycardia, tachypnea, and abdominal fullness.
DIAGNOSIS OF SICKLE CELL ANEMIA
Clinical …….80% of cases.
Laboratory diagnosis:
Electrophoresis…cellulose acetate
DIAGNOSTIC METHODS INCLUDE:
Full blood count, blood film and reticulocyte count, bilirubin.
Hb electrophoresis using cellulose acetate or agar gel
High-performance liquid chromatography (HPLC)
Isoelectric focusing (IEL)
Polymerase chain reaction (PCR)
Supplementary genetic tests
MANAGEMENT FOR A STEADY-STATE
Determine and record physical/Haematol Parameters.
Avoid factors that encourage sickling.
Folic acid supplementation.
Malaria prophylaxis.
Treatments
ANTISICKLING AGENTS
Hydroxycarbamide, formerly known as Hydroxyurea.
15mg/kg/24 hrs. gradually increase to max of 30mg/kg/24hrs. Monitor FBC, LFT and HbF. Increase in HbF is usually 10-15%
Trade name –Hydrea
*5-Azacytidine,
*decitibine
*Histone deacetylase inhibition: short-chain fatty acids –butyric acid.
*Recombinant human erythropoietin (rhEPO)
It is important to note that hydroxycarbamide is the most successful drug therapy for scd.
It is a cytotoxic and cytoreductase antimetabolite that acts via inhibition of DNA synthesis by inhibiting ribonucleotide reductase. Known pharmacological effects that may contribute to the drug’s efficacy in SCD include:
Hydroxycarbamide
1.increase in red cell content of Hb F.
2.dose related cytoreductase effects on neutrophils.
3.increase in water content of red cells.
4.increased deformability and successful microvascular navigation of sickled cells.
5.altered adhesion of RBCs to endothelium by decreasing the expression of endothelial adhesion molecules.
Treatment with hydroxycarbamide shows significant reduction in bone pain crises, admissions, and need for blood transfusion#
Gene therapy
The term gene therapy is applied to any maneuver in which genes or genetically modified cells are introduced into a patient for therapeutic benefit. Gene therapy corrects sickle cell disease in mice, scientists report therapies designed to treat genetic disease in humans.
The therapy transfers an anti-sickling variant of the faulty gene to the bone marrow, where it incorporates itself into the stem cells that give rise to red blood cells. In two mouse models, the new gene was rapidly expressed in 99 percent of all circulating red blood cells, preventing sickling and other signs of the disease, Leboulch said.