In the pathophysiology of Sickle cell anemia or Sickle cell disease (SCD), we learn
Continue reading
…creating a healthy world

In the pathophysiology of Sickle cell anemia or Sickle cell disease (SCD), we learn
Continue reading
The pathophysiology of scabies is worthwhile and everyone ought to know the cardinal symptoms
Continue reading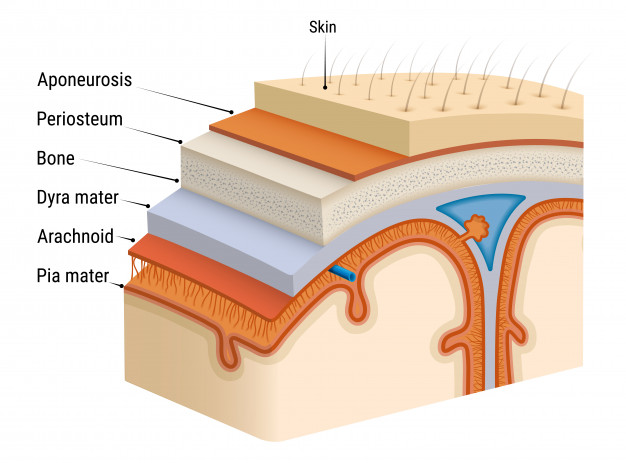
let’s take a look at Meningitis pathophysiology and other essential things for a better
Continue reading
Let’s take a look t the pathophysiology of HIV and the important facts to
Continue reading
The pathophysiology of Syphilis is worth knowing, and a great concern for many in
Continue reading
The pathophysiology of chlamydia comes with many questions, and in this article, it will
Continue reading